How pathophysiology of heart disease impacts outcomes?
How pathophysiology of heart disease impacts outcomes?
Introduction
In the year 2016, famous Telugu actor Chiranjeevi underwent angioplasty, and has been leading a normal life ever since. During a routine check-up, Chiranjeevi learnt of possible heart issues, and followed up with timely intervention. Lets take a good look at pathophysiology of heart disease and its impact on the effectiveness of treatment.
A brief outline of rheumatic heart disease pathophysiology?
Rheumatic heart disease refers to a chronic condition due to rheumatic fever post Streptococcus infection. To continue with an understanding of pathophysiology of heart disease, let’s look at RHD in better detail.
- Streptococcal Infection – Typically, RHD begins with throat infection due to Group A Streptococcus bacteria. Following this, the body’s immune response system works starts working.
- Autoimmune condition – People who have autoimmune conditions, will end up with the immune system attacking own tissues, such as the heart, joints, skin, and central nervous system.
- Acute Rheumatic Fever – Due to extensive inflammation affecting the heart, this causes rheumatic carditis.
- Valve damage – Due to inflammation of the heart valves, and damage, the valves either do not open as required or close as required, affecting blood flow to the heart.
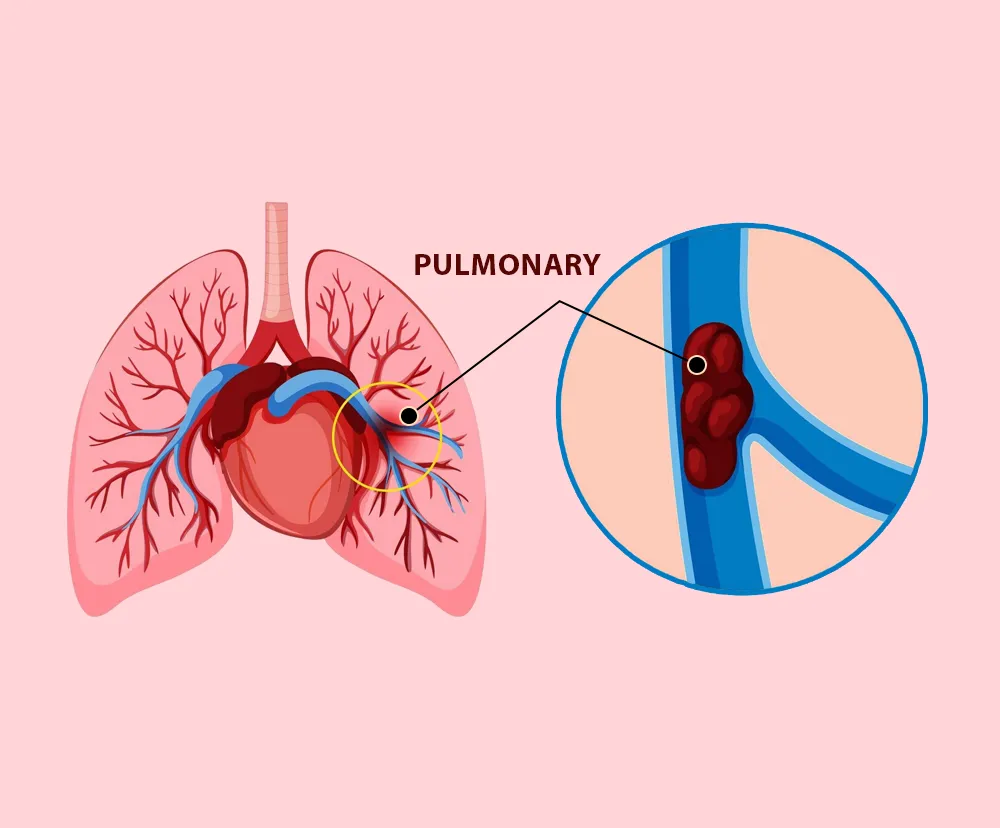
- Progression – Due to increased workload from valve dysfunction, the heart may end up enlarged. Additionally, formation of blood clots can result in a possible stroke.
RHD is a condition that will remain forever, and requires to be managed. This may involve surgery on the damaged valves.
What is pathogenesis of rheumatic heart disease?
Pathogenesis of rheumatic heart disease refers to the manner in which RHD develops and progresses. The whole context of this article is the pathophysiology of heart disease and includes the symptoms and outcomes. This will help in choosing the best treatment and approach to intervention. This will also help in identifying the symptoms to conclusively confirm or rule out the disease.
RHD is due to a complex combination of infections, immune response, and inflammatory conditions. All of this cause chronic damage to the heart valves, and this impacts the flow of blood to the heart. A preventive approach would include use of antibiotics for timely treatment of streptococcal pharyngitis. By preventing and managing streptococcal infections it is possible to pre-empt the autoimmune and inflammatory actions that cause chronic heart valve damage.
What is pathophysiology of congenital heart disease?
Congenital heart disease is the result of structural defects in the heart or certain blood vessels at the time of birth. This affects the functioning of the heart and would result in severe outcomes depending on the nature of the defect. As part of the effort to understand the pathophysiology of heart disease here is a detailed look.
- Genetic component – A lot of congenital heart defects are due to genetic mutations that are either inherited or occur during fetal development. Common genetic syndromes include Down syndrome, Turner syndrome, and DiGeorge syndrome.
- Environmental reasons – Apart from the above, maternal infections such as rubella, or use of drugs, alcohol consumption during pregnancy can cause CHD. Diabetes during pregnancy can also cause CHD.
Different types of congenital heart defects
The different types of CHD include the following:
- Acyanotic heart defects.
- Septal defects.
- Patent Ductus Arteriosus.
- Coarctation of the aorta.
- Valvular defects.
- Cyanotic heart defects.
- Tetralogy of fallot.
- Transposition of the great arteries.
- Truncus Arteriosus.
- Total Anomalous Pulmonary Venous Return.
Possible symptoms include the following:
- Discoloration of the skin, lips or mucous membranes.
- Heart murmurs.
- Heart failure.
- Development issues.
The condition can be managed through medications, surgical procedures, and monitoring. A better understanding the underlying conditions helps in improved diagnosis, treatment, and outcomes.
What is meant by etiology of rheumatic heart disease?
Etiology refers to the origin of a disease, and RHD etiology can be considered as a part of pathophysiology of heart disease. Lets look at the key factors that influence the disease, and have a bearing on the outcomes of treatment.
The primary cause, as mentioned above, is due to strep throat, an infection. Post infection, the immune system of the body mounts a response and may end up harming the body’s own tissues, especially the heart. RHD is relatively more prevalent among low income and middle-income group people. This is mainly due to overcrowding, lack of healthcare, and poor treatment of streptococcal infections.
Diagnosis of rheumatic heart disease and role of genetic testing
While genetic testing offers analysis about future or lifetime risk of heart disease, its role in diagnosis of rheumatic heart disease is indirect and not the standard test. As seen above, RHD is due to infections, and the body’s response to the infections. Therefore, the genetic component is limited. However, there are two areas where genetic testing can help:
- Some people are genetically predisposed to having severe reactions to strep throat infections. This can be detected through genetic testing.
- Auto immune conditions are also a factor in RHD. Genetic testing can help reveal if the person has any auto immune condition. This can help understand the person’s possible response to any condition.
Therefore, genetic testing does not have a direct role in detecting RHD in patients. However, it can help in understanding certain conditions that could be causative factors for future RHD. Genetic testing facilities in Tamil Nadu presently offer advanced testing services to check for future or lifetime risk of heart disease.
The tests are relatively simple, with blood or saliva samples used for analysis. A detailed analysis of the sample helps in understanding genetic mutations and inherited conditions that will give a clear picture of future or lifetime risk of heart disease.
Based on the analysis and reports, intervention in the form of medications and lifestyle changes can reduce the risk considerably. In some instances, surgical procedures can correct problems and prevent the risk of heart disease. Intervention can help reduce the effects of any possible cardiovascular event in the future, thereby saving lives and improving the quality of lives.
Related Blogs :

Do any of these risk factors for heart disease apply to you?
Do any of these risk factors for heart disease apply to you? Introduction Measures required for coronary heart disease prevention. What is the connection between diabetes and...

Why it is important to treat rheumatic heart disease with a sense of urgency?
Why it is important to treat rheumatic heart disease with a sense of urgency? Introduction What is pulmonary heart disease? What is rheumatic valvular heart disease? What...

Education: Master of Public Health (MPH) from the Postgraduate Institute of Medical Education and Research (PGIMER), Chandigarh Experience: A dedicated health writer with 8 years of experience covering a range of health topics, including public health and nutrition. His work has appeared on reputable Indian health websites and journals such as India Health Journal and The Health Times. Ravi also collaborates with Indian health agencies on public health campaigns.