
Is Addiction in Your Genes? The Truth Might Shock You!
- Addiction Risks: Family History Is More Than a Coincidence
- Which Genes Play a Role in Addiction Risk?
- Alcoholism and Genetic Susceptibility
- Early Use and Genetic Triggers of Addiction
- Addiction Risks Are Multilayered
- Why Some People Stay Addicted Longer
- Can Genetic Testing Help with Addiction?
- DNA Alone Does Not Determine the Destiny of Addiction
- Genetic Testing: Where to Start If You’re Concerned
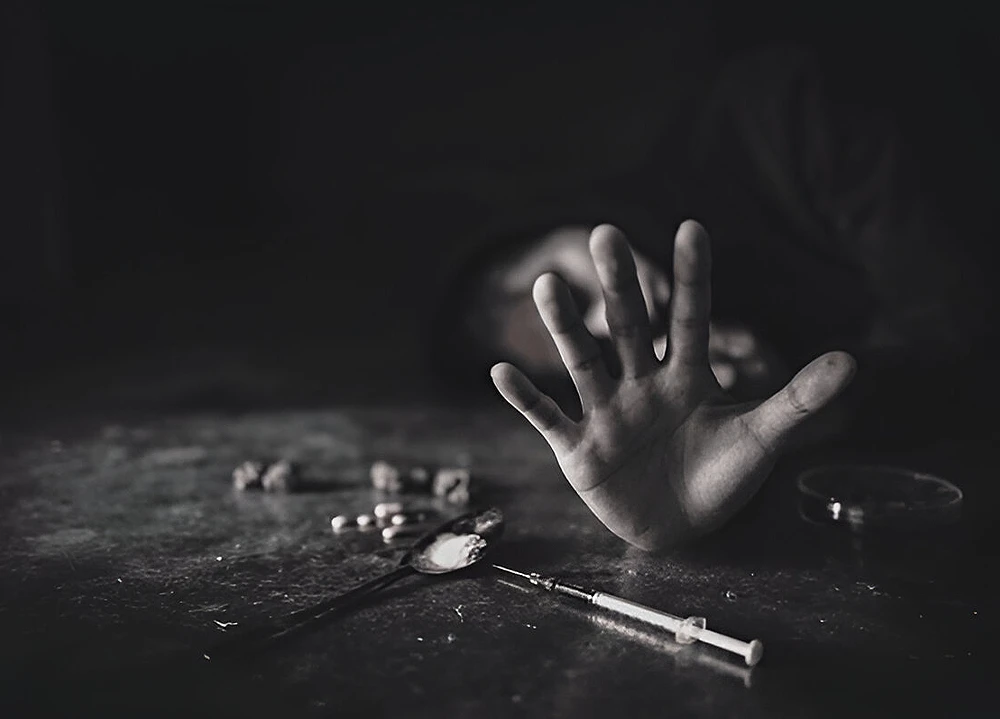
Genetic science has begun uncovering a hard reality: that addiction risk is partly inherited. What once looked like a pattern of bad choices now maps back to biology. People with certain DNA variations may experience stronger cravings, faster dependence, and reduced response to standard treatments.
These traits are measurable, and the research continues to evolve.
For families with a long history of substance misuse, this raises urgent questions. Are some people genetically wired to lose control? Can addiction run through bloodlines without anyone realizing the link? And if so, what can be done about it?
Addiction Risks: Family History Is More Than a Coincidence
The numbers speak clearly. According to data from the Orlando Recovery Center, individuals with an addicted parent are “eight times more likely to develop a substance use disorder compared to those with no family history.” Siblings of those with alcohol dependence face elevated risk even after accounting for shared environment.
Genes contribute to that trend. Twin and adoption studies consistently show that biological relatives of addicted individuals are more likely to develop the same issues, even when raised apart. This means that something hard-coded into DNA is playing a role.
So, it is important to note that:
- Early exposure to substances tends to occur more frequently in families with an addiction history, increasing the likelihood of habitual use during adolescence.
- Children of addicted parents often inherit differences in stress response genes, which influence coping behavior under pressure.
- Neurodevelopmental traits like impulsivity or risk-seeking behavior often run parallel to addiction in genetically linked families.
- Patterns of poor sleep regulation, commonly tied to addiction risk, have been found to cluster in certain family bloodlines.
- Families with a history of substance misuse often display higher rates of mood instability, further reinforcing genetic susceptibility.
Which Genes Play a Role in Addiction Risk?
Dopamine Receptor Genes (DRD2)
The DRD2 gene affects how dopamine receptors function. Certain inherited variants can reduce receptor density, which lowers the brain’s natural response to rewarding experiences. This change can lead individuals to seek external stimulation—such as drugs or alcohol—to fill that gap.
GABA-Related Genes (GABRA2)
GABRA2 influences the regulation of inhibitory signals in the brain. Variants in this gene have been linked to lowered impulse control and greater sensitivity to stress, both of which are connected to higher addiction vulnerability.
Opioid Receptor Genes (OPRM1)
OPRM1 controls how the brain responds to opioids. Inherited changes in this gene can alter pain relief, emotional response, and drug tolerance. People with certain OPRM1 variants often report stronger cravings and more difficulty managing use.
Dopamine Transporter Genes (SLC6A3)
SLC6A3 plays a role in clearing dopamine from the brain after it has been released. Mutations here can affect how long reward signals stay active. Some versions of this gene are associated with stimulant sensitivity and compulsive behaviors.
Genetic pathways shared across substances
A 2023 NIH study identified shared genetic markers across multiple types of addiction. These include substances such as nicotine, alcohol, opioids, and stimulants, which all interact with the brain’s reward and learning circuits in genetically similar ways.
Alcoholism and Genetic Susceptibility
The connection between alcohol dependence and genetics is well-documented. Studies estimate that up to 60% of alcohol use disorder risk is linked to genetic factors. Variants in ADH1B and ALDH2, two genes responsible for alcohol metabolism, influence both how alcohol is processed and how severely someone experiences withdrawal.
People of East Asian descent often carry versions of ALDH2 that slow alcohol breakdown, leading to strong physical reactions. Ironically, this can reduce alcoholism risk due to discomfort. In contrast, people with faster-metabolizing versions may drink more frequently before feeling any effects, raising dependence risk.
Early Use and Genetic Triggers of Addiction
Genetic risk interacts with the age of first exposure. Early drug or alcohol use during adolescence, when the brain is still developing, raises the chance of addiction, especially in those with inherited vulnerabilities.
Research showed that genetic variations in the brain’s learning and reward circuits increase sensitivity to early substance exposure. Individuals with those traits tend to escalate use rapidly and experience stronger cravings, even when initial exposure was brief.
Addiction Risks Are Multilayered
Genes rarely act alone. The interaction between genetic variants and stressors determines who moves from use to dependence. According to a 2022 study, addiction risk can rise steeply when genetic markers overlap with trauma history, untreated anxiety, or poor sleep regulation.
This complexity has made prediction difficult. However, gene-wide association studies continue to reveal new combinations that elevate risk across several behaviors like gambling, binge drinking, compulsive eating, and drug misuse.
Other contributing factors also shape this progression:
- Social isolation can heighten the impact of inherited dopamine pathway variations, pushing individuals toward substances for stimulation.
- Epigenetic shifts caused by early drug exposure may activate dormant risk genes, increasing susceptibility over time.
- Coexisting attention or mood disorders often interact with reward-related genes, raising the probability of substance-seeking behavior.
- Hormonal imbalances during adolescence can amplify genetic vulnerabilities tied to impulse and stress regulation.
Why Some People Stay Addicted Longer
Inherited traits affect more than initiation. They also shape how addiction behaves over time. Variants in CYP2A6 and CYP2B6, which govern how drugs are metabolized, can slow detox and intensify withdrawal symptoms. This makes relapse more likely and treatment harder to sustain.
A review found that some individuals with these metabolic traits struggle with conventional dosing in rehabilitation programs. Their bodies hold substances longer, increasing side effects and complicating recovery.
Others lack the protective gene expressions that modulate anxiety and impulse. Without those natural brakes, cravings last longer and return faster.
Can Genetic Testing Help with Addiction?
Risk identification before first use
Testing for addiction-related mutations is growing. While it cannot predict behavior perfectly, it does highlight high-risk pathways that inform prevention and treatment. According to a study, identifying these markers early can help families plan support strategies before drug or alcohol use begins.
Support for high-risk adolescents
This kind of screening may be especially valuable for teens with a strong family history. Understanding inherited vulnerabilities can guide earlier interventions, stronger boundaries, and closer monitoring during key developmental stages.
Guidance for relapse-prone adults
Adults entering recovery after multiple relapses may benefit from insights that explain why certain treatments failed. Genetic screening can direct care toward options that match the body’s internal biology.
DNA Alone Does Not Determine the Destiny of Addiction
Genes influence risk. They do not decide the outcome. People with high-risk mutations can still live substance-free lives. The difference often lies in awareness, structure, and support.
That means early intervention, routine screening, and informed care plans still matter even for those born with biological vulnerabilities.
Genetic Testing: Where to Start If You’re Concerned
If addiction shows up repeatedly in your family history, the next step is education. Learn which traits tend to cluster. Consider speaking to a genetic counselor. Look at your own responses to stress, reward, and compulsive behavior. These patterns often appear long before drugs or alcohol enter the picture.
For those who want a clearer view, Lifecode offers a full addiction risk screening kit. You collect a sample at home and return it by mail. The lab checks for dozens of genetic variants tied to drug, alcohol, and behavioral addiction. Your report is reviewed by a Lifecode counselor who explains what your results mean and how to move forward.
This test won’t change your DNA. But it could change how you respond to it. Start with knowledge. Then make the choice to act early.

Can You Inherit Migraine Risk The Truth About Women’s Brain Health
Can You Inherit Migraine Risk The Truth About Women’s Brain Health The Genetic Link to Migraines, It Is More Than Just Bad Luck Why Women are More...


Unlocking Your Body’s Blueprint: Genetic Clues to Pregnancy Complications and Hypertension
Unlocking Your Body's Blueprint: Genetic Clues to Pregnancy Complications and Hypertension The Intricate Dance of Genes and Health Decoding Pregnancy Complications Through Genetics The Genetic Roots of...

Education: Bachelor of Pharmacy (B.Pharm) from the Tata Institute of Social Sciences (TISS), Mumbai Experience: Agarwal is a seasoned pharmacist with over 7 years of experience in the pharmaceutical field. She has worked in various settings, including hospital pharmacies and community clinics, where she has excelled in medication management, patient counseling, and clinical support. Agarwal is known for her expertise in drug therapy optimization and patient safety. In addition to her practical experience, she contributes to health journalism, focusing on pharmaceutical advancements and health policy, and is involved in research projects aimed at improving medication practices and health outcomes. is known for her expertise in drug therapy optimization and patient safety. In addition to her practical experience, she contributes to health journalism, focusing on pharmaceutical advancements and health policy, and is involved in research projects aimed at improving medication practices and health outcomes.


