Cancer chemotherapy
Cancer chemotherapy
Introduction
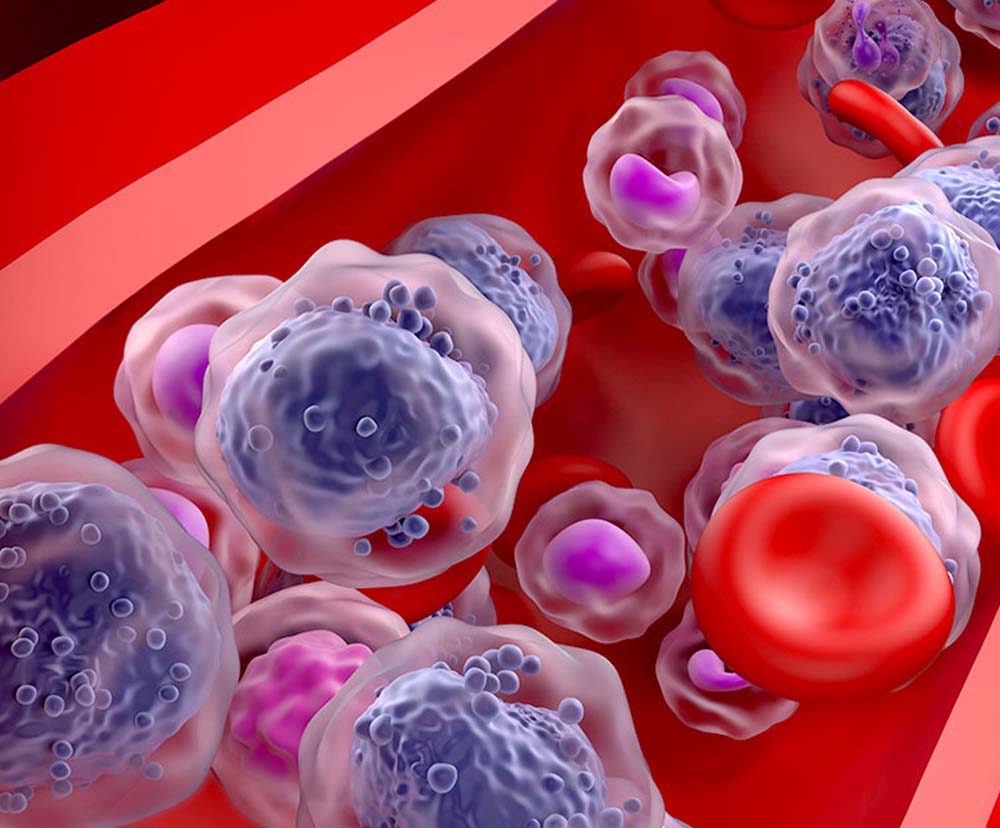
Chemotherapy works by administering anti-cancer meds to damage cancerous cells or inflict damages onto such harmful / rapidly growing cells. Almost all of these drugs offered through chemotherapy are known to function in distinctive cycles or stages. This means – meds under chemotherapy work uniquely upon those having cancer. Caregivers understand these phases and what drugs work best for the treatment of cancerous conditions.
So, what is chemotherapy for cancer?
Meds used as part of chemotherapy do not isolate triggers that cause cancers; they cannot tell healthy or harmless cells from cancerous ones. Owing to this, several harmless cells also can get injured by chemo meds.
Caregiving teams aim at lessening the injuries of healthier or harmless cells; the team also strives to increase damages caused to fast-spreading, cancerous tissues and cells. In general, you need not panic about damages or injuries inflicted to healthy cells or harmless ones. Your harmless cells – upon being damaged – get back to life and pursue their normal functions in due course of time. Thus, chemo meds rarely trigger damages to active and healthy cells.
You need to know chemotherapy is a time-tested and a trusted route for the treatment of cancer. This route comprises the use of potent anti-cancer drugs. Many meds – more than 100 of them – do have the approval of the federal drug agency – Food & drug administration (FDA). All drugs used under chemotherapy aim to accomplish either of these 2 tasks – add more life to the person living with cancers or cure their autoimmune problem.
At what stage is chemotherapy used?
Of the available modes of treating cancers, chemotherapy is administered at almost all stages of this autoimmune condition.
At the preliminary stages, chemo meds are offered for curing the growth of cancerous cells. But, if the cancerous condition has started to spread to nearby tissues or sites, chemotherapy is used for offering palliative care.
At the stage–1, this modality is used on a trial post-surgery. But at stages 2, chemotherapy is either preceded or followed by a surgical procedure. Among those with 3A stage of cancer, cancers are mostly treated through a surgical approach. Here, chemo drugs are offered with radiation therapies and / or surgeries.
If cancers are in 3A stages – these are not removed through surgical means; instead, chemo drugs are provided along immunotherapy or with radiation therapy. In 3B and 3C stages of cancers, chemo drugs are provided with extra sittings of radiation treatment. In a few remote instances, this combinatorial treatment is followed by radio-sensitised treatment modalities.
For stage 4 of cancers, chemo meds are offered together with targeted therapy. If you witness a relapse of cancers, chemo drugs are provided with additional sittings of chemotherapy.
Is chemotherapy painful?
Foremost of all, administration of chemo meds is not a discomforting protocol. However, pains are part of the usual set of side effects, experienced during most sittings of chemotherapy. Each sitting involves delivery of drugs intravenously; these may consume not more than 4 minutes per sitting. A caregiver – often, a medical specialist administers meds through a catheter into your vein(s). In most cases, veins of the arm are chosen to deliver these meds. Oncologists may use a tube of a very thin radius – also called a catheter. Through this slim tube, drugs gain entry inside the system.
Those who are taking chemotherapy may feel painful sensations; these pains show up right at the site where drugs are delivered into the body. Most painful sensations tend to go away once the medical oncologist removes the needle or catheter. Needles are taken off quickly after a sitting gets completed. In some instances, catheters or needles known as ‘ports’ are left to stay on your system. These may be left there for a sizable span of time. This helps reduce the need to insert the catheter multiple times; it also serves to deliver many forms of drugs during a single cycle of treatment.
Apart from intravenous delivery of drugs, a few meds are also taken in their ‘pills’ form or as tablets. Such pills are taken orally. You may need to swallow them with 8 to 9 ounces of potable water. You are unlikely to feel a pain when you are ingesting these tablets.
Chemotherapy before and after
Before the start of each chemo sitting, it is a good practice to know more of the meds administered. Often, the pack of meds used include those which destroy cancerous cells; the pack may also include meds that can alleviate painful feelings. It is equally important to know how long each session will consume; a few sittings can take some hours. However, there are some which may need less than 5 minutes’ time.
The entire chemotherapy treatment plan may require 5 to 7 weeks of your time. It can be of great use to have a friend accompany you during these sittings.
There are also a few drugs that are taken prior to start of chemotherapy sittings. Hence, taking a pal or chum with you can help handle the side effects of these drugs. More often, meds taken prior to start of chemotherapy sittings can kick in a feeling of tiredness or fatigue. Having a pal by your side enables you to pass time with relative ease; this is because sitting in the healthcare facility – all alone – can be quite tiring.
Tell your friend to watch out for undesired effects such as giddiness, flushing, inflammation or bruising; your friend may seek assistance from the treating doctor or caregiver as soon as these adverse effects erupt.
Prio to each chemotherapy sitting, it is essential to drink adequate amounts of water or such other liquids like juices. You however need to avoid caffeinated drinks like tea or coffee. It is safe to stay away from soda or other carbonated beverages.
Staying hydrated is an important thing to do: this is chiefly due to meds given for cancers can dry you up. Taking enough amounts of fluids can help reduce incidence of headache, fatigue and dizziness. It is a safe thing to drink at least 9 ounces of fluids (like water) each hour after every sitting of chemotherapy. It is equally important to refrain from taking caffeinated drinks. Intake of water can help in keeping you hydrated.
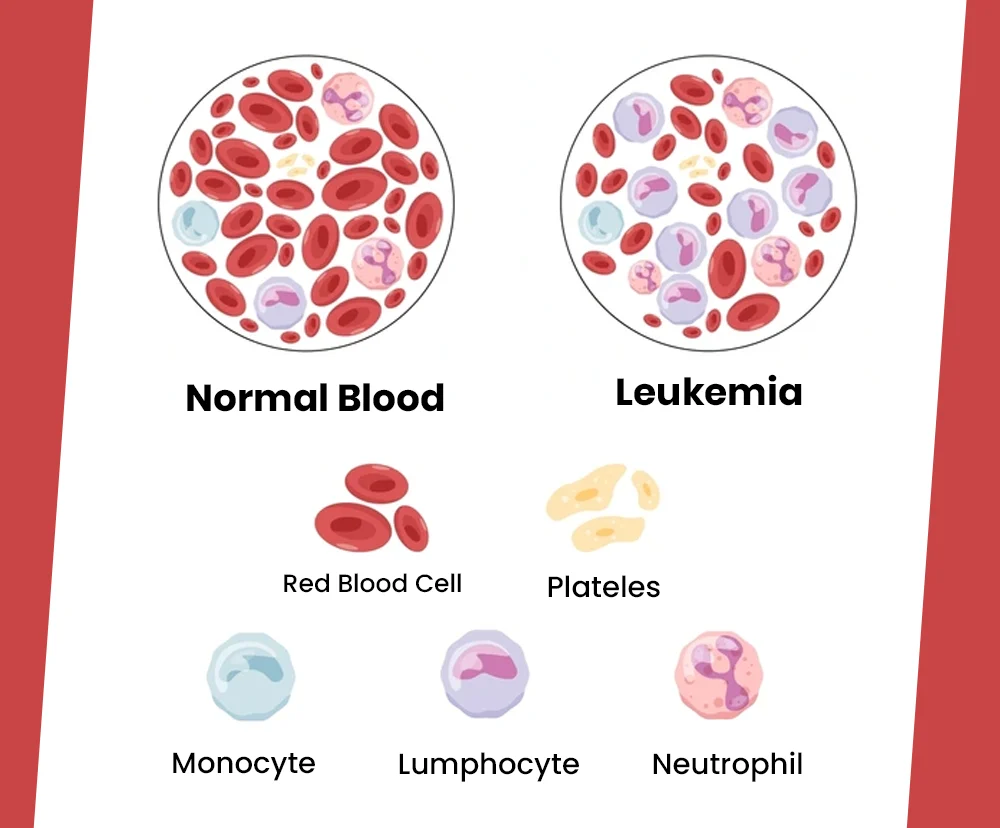
You may also need to anticipate likely adverse outcomes like abdominal pain, vomiting, spells of insomnia, pains, loss of scalp hair, significant reduction in cells of your blood, etc. Most of these can affect other organs of your body – for instance, the central nervous system i.e., CNS may get affected. So, ensure to tell your treating doctor of losing your imbalance, lack of bodily coordination, involuntary shaking of body, muscular pains, etc.
Lastly, prior to chemotherapy sittings, the caregiving team will make you take a blood count test – known as complete count of blood cells. The outcomes of this test will let understand the count of blood cells i.e., red blood cells, white cells as well as platelets. This works as a basis to understand the impact of chemotherapy sittings on your blood.
After chemotherapy
Experiencing pains is a common side effect of chemotherapy, and also of other forms of cancer treatments. You may witness pains in the form of numbness or as a burning sensation. In a few instances, people have experienced acute spells of pains. Most of these discomforts may show up in your hands and legs.
In general, pains are categorised under neuropathy related discomforts. These pains may occur owing to injuries of nerves – caused by meds or due to rapid multiplication of cells. Most people may also see pains like severe / splitting headache, pain in your lower abdomen as well as painful joints or muscles. Pains can however be treated. There are a few types of painkilling meds used for this purpose. But all these meds need to be taken under the advice of a qualified medical professional.
If you are experiencing unbearable levels of pains, your treating team may recommend a few other alternative routes to manage such discomforts. These can include approaches like deep spells of respiration, acupressure, physical therapy, hypnosis as well as bio feedback sessions. In order to have more details, it is a good practice to speak with your treating physician.
It is a recommended to have a journal to record severity of your pains, experienced throughout the treatment process. Take needful support from the caregiving team each time painful sensations disrupt your daily walk of life.
Related Blogs :

Leukemia Blood Test
Leukemia Blood Test Introduction Blood test for leukemia Leukemia diagnosis blood test Leukemia blood test results Leukemia cancer CBC blood test results Leukemia positive cancer blood test...

Chronic myeloid leukemia
Chronic myeloid leukemia Introduction Chronic myeloid leukemia ICD 10 What is chronic myeloid leukemia? Chronic myeloid leukemia symptoms Chronic myeloid leukemia treatment Introduction Tissues of the marrow...

Education: Bachelor of Pharmacy (B.Pharm) from the Tata Institute of Social Sciences (TISS), Mumbai Experience: Dr. Agarwal is a seasoned pharmacist with over 7 years of experience in the pharmaceutical field. She has worked in various settings, including hospital pharmacies and community clinics, where she has excelled in medication management, patient counseling, and clinical support. Dr. Agarwal is known for her expertise in drug therapy optimization and patient safety. In addition to her practical experience, she contributes to health journalism, focusing on pharmaceutical advancements and health policy, and is involved in research projects aimed at improving medication practices and health outcomes. is known for her expertise in drug therapy optimization and patient safety. In addition to her practical experience, she contributes to health journalism, focusing on pharmaceutical advancements and health policy, and is involved in research projects aimed at improving medication practices and health outcomes.